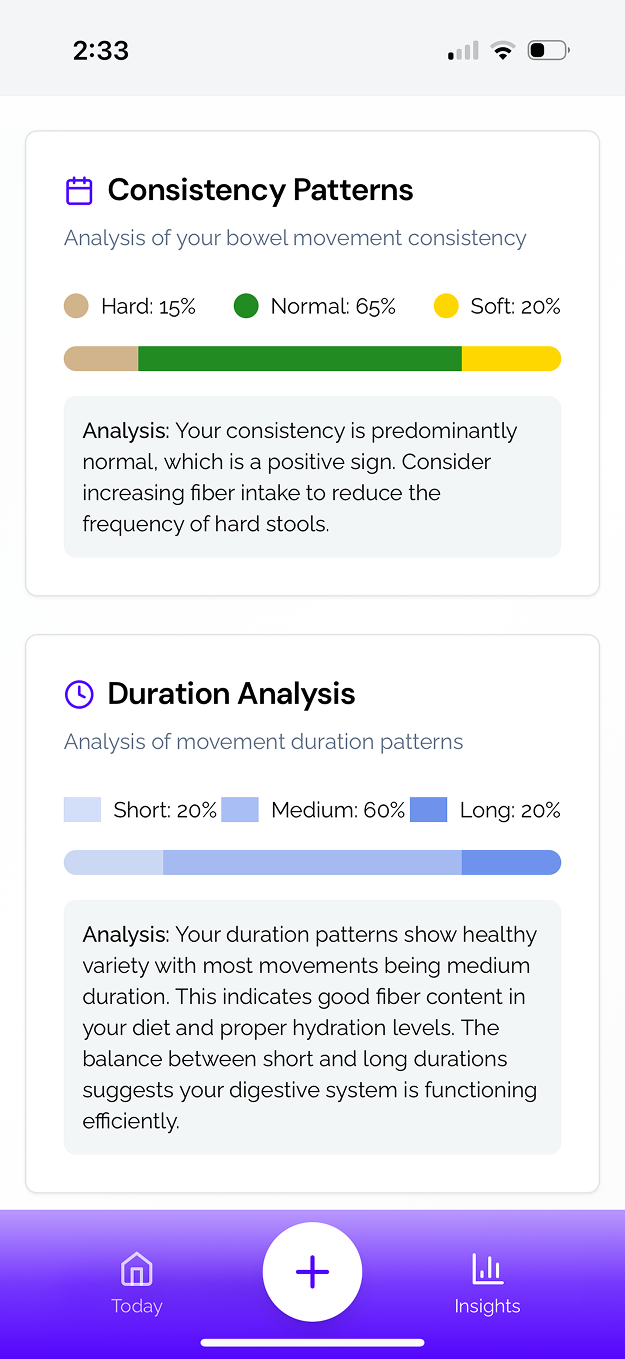
Food Sensitivity Detection Through Advanced Gut Health Tracking
Stop guessing with your diet. Learn how real-time microbiome tracking identifies food triggers and builds lasting tolerance.

Food sensitivity is not fixed. It evolves with your gut health, stress levels, sleep quality, and overall lifestyle. Many people spend years cycling through elimination diets and inconsistent test results without realizing the true problem — they are chasing a moving target.
With advanced gut microbiome tracking, you can identify your food triggers in real time, measure your personal tolerance levels, and replace months of guesswork with data-backed insights. This approach does not just avoid problem foods — it actively works to restore your tolerance and expand your diet.
Why Traditional Food Sensitivity Testing Often Misses the Mark
1. IgG Testing Limitations
IgG antibody tests measure immune exposure to a food, not whether that food is actively causing symptoms. A high IgG response might simply indicate regular consumption rather than a harmful reaction.
2. Elimination Diet Challenges
An elimination diet is often the default recommendation for suspected food sensitivity. While useful in some cases, it can be:
- Time-consuming, requiring weeks or months of strict food restriction
- Psychologically difficult, leading to food anxiety or social limitations
- Inconclusive if multiple variables change at once
3. Food Diary Subjectivity
Keeping a symptom log or food diary relies on memory and self-reporting. Delayed reactions, subtle symptoms, and lifestyle factors make it hard to draw accurate conclusions.
4. Lack of Personalization
Most advice on food sensitivities is generic, ignoring how your unique gut microbiome and bacterial diversity influence food processing and tolerance. Two people can react completely differently to the same food, even with similar symptoms.
Real-Time Food Sensitivity Detection with Gut Microbiome Tracking
Your gut microbiome responds to food within hours. By capturing data immediately after eating, you can pinpoint the exact foods or combinations that cause problems.
Advantages include:
- Precise trigger identification without relying on guesswork
- Dose-response mapping to find your personal thresholds
- Interaction detection for food combinations that worsen symptoms
- Dynamic tracking of sensitivities over time
- Context awareness that links symptoms to factors like sleep, stress, and hydration
Example: If a microbiome analysis shows an increase in gas-producing bacteria after eating lentils, combined with symptom tracking, you can confirm whether lentils are a true trigger or only problematic when combined with other foods.
Common Food Sensitivity Patterns in Microbiome Data
FODMAP Intolerance vs. True Sensitivity
FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are carbohydrates that can cause digestive distress in some people. Many cases of “food sensitivity” are actually temporary digestive health issues caused by:
- Missing bacteria needed to ferment certain fibers
- Overgrowth of gas-producing bacterial strains
- Low microbial diversity reducing fiber tolerance
Gut health tracking helps identify whether your FODMAP reactions are due to true sensitivity or an imbalance that can be corrected.
Dairy and Lactose Reactions
Some dairy reactions are the result of low lactase enzyme activity, while others are linked to microbiome composition. Adding fermented dairy (like kefir or yogurt) or lactase enzymes can sometimes restore tolerance.
Histamine Reactions
Histamine sensitivity can be influenced by gut bacteria that produce or break down histamine. Tracking can reveal patterns where symptoms appear after eating aged cheeses, fermented foods, or wine, especially in combination with stress or poor sleep.
The Food Sensitivity Context Matrix
Food reactions are rarely caused by a single food in isolation. The Food Sensitivity Context Matrix helps explain why a food might trigger symptoms on one day but not another.
Factors include:
- Previous meals: The meal before can alter gut bacteria activity, changing your reaction.
- Stress levels: High stress can weaken gut barrier integrity, making you more reactive.
- Sleep quality: Poor sleep affects immune regulation and gut motility.
- Gut barrier integrity: Increased permeability (“leaky gut”) can allow larger food particles to trigger inflammation.
- Bacterial diversity: More diverse microbiomes are better at breaking down a wide range of foods.
Example: You may tolerate sourdough bread after a restful night but react after a stressful day with poor sleep, even though the food is identical.
The Sensitivity Spectrum Approach
Traditional elimination diets often frame foods as “safe” or “unsafe.” In reality, most food sensitivities exist on a spectrum.
Advanced gut health tracking can help you discover:
- Personal thresholds: How much of a food you can eat without symptoms
- Timing strategies: Certain foods may be better tolerated earlier in the day
- Preparation methods: Cooking, soaking, fermenting, or sprouting can reduce reactivity
- Supportive pairings: Combining challenging foods with gut-friendly choices can lower symptom risk
This spectrum-based view allows you to gradually rebuild tolerance rather than permanently restrict foods.
The Smart Elimination Protocol
Instead of cutting entire food groups for months, use a personalized elimination process:
- Baseline Assessment
- Eat a consistent, low-reactivity diet for 1–2 weeks
- Track symptoms, sleep, stress, and activity
- Run an initial microbiome analysis to understand your bacterial diversity and digestive biomarkers
- Single-Food Challenges
- Introduce one food at a time, in a controlled portion
- Monitor symptoms and microbiome shifts over the next 48–72 hours
- Objective Response Measurement
- Use microbiome tracking to confirm bacterial or metabolite changes
- Compare against baseline readings
- Threshold Testing
- Gradually increase portions to find your tolerance limit
- Mapping and Adjustment
- Build a personalized tolerance map for each potential trigger
- Dynamic Reintroduction
- Re-test foods periodically as gut health improves
Healing vs. Avoidance: The Long-Term Solution
Avoidance can temporarily control symptoms, but it does not address the root cause. A healing-focused strategy aims to expand your diet over time by:
- Improving bacterial diversity with a variety of plant fibers and fermented foods
- Repairing the gut barrier with anti-inflammatory nutrients and lifestyle changes
- Reducing gut inflammation through stress management and restorative sleep
- Gradually reintroducing foods using controlled challenges
Practical Tips for Managing Food Sensitivities While Healing
- Start with low-FODMAP versions of challenging foods
- Use fermented preparations (e.g., sauerkraut, sourdough) to improve digestibility
- Keep servings small at first, then build up
- Combine trigger foods with soothing, nutrient-dense choices like bone broth or cooked vegetables
- Avoid testing new foods during high-stress periods
- Maintain a symptom and context log alongside microbiome data
Sample 8-Week Food Sensitivity Optimization Plan
Weeks 1–2: Baseline & Stabilization
- Simple, low-reactivity meals
- Track all relevant lifestyle variables
- Initial microbiome testing
Weeks 3–4: Targeted Food Challenges
- Test one food every 3–4 days
- Measure microbiome and symptom changes
Weeks 5–6: Dose & Interaction Mapping
- Experiment with portion sizes and food combinations
- Use preparation methods to improve tolerance
Weeks 7–8: Review & Reintroduction
- Update tolerance map
- Expand diet strategically based on results
What to Track for Reliable Results
Objective Metrics:
- Microbiome diversity scores
- Bacterial abundance for key digestive strains
- Short-chain fatty acid production
- Gut inflammation markers
Subjective Metrics:
- Symptom type, severity, and timing
- Energy levels, mood, and cognitive clarity
- Stress and sleep quality
Combining both types of data ensures you are making changes based on measurable outcomes, not just perceptions.
When to Seek Professional Guidance
Severe reactions (such as swelling, difficulty breathing, or rapid heartbeat) require immediate medical attention. Chronic or unclear symptoms should be evaluated by a healthcare professional familiar with microbiome-based assessment and digestive health tracking.
Related Resources
- Food Sensitivity vs. Food Allergy: How Gut Health Tracking Reveals the Truth
- Beyond Elimination Diets: Smart Food Sensitivity Detection Methods
- The Hidden Food Triggers Your Gut Health Data Will Reveal
- How to Heal Food Sensitivities Instead of Just Avoiding Trigger Foods
- Real-Time Food Sensitivity Tracking: The End of Guesswork Dieting
Key Takeaways
- Food sensitivity is dynamic and influenced by gut microbiome composition, lifestyle, and environment.
- Traditional testing and elimination diets often fail because they lack objective, real-time feedback.
- Gut health tracking with microbiome analysis allows for precise trigger identification, tolerance mapping, and long-term healing.
- The goal is not permanent restriction, but improved digestive health and expanded food freedom.
Other Posts
Be first to try SNIFR. Beta coming soon.
Join our waitlist to get notified when the app launches. Start understanding your gut health sooner.