Advanced Digestive Monitoring: Transforming Management of IBS and Gastrointestinal Diseases
Revolutionary digestive monitoring technology delivers real-time IBS insights and personalized GI disease management through advanced data analysis.

The Gastrointestinal Disease Landscape
Gastrointestinal (GI) diseases affect an estimated 60-70 million Americans annually, with conditions ranging from common functional disorders like Irritable Bowel Syndrome (IBS) to inflammatory conditions such as Crohn's disease and ulcerative colitis. These digestive health challenges create substantial physical, emotional, and economic burdens for patients. Traditional diagnostic approaches for gastrointestinal diseases rely heavily on subjective symptom reporting, delayed laboratory results, or invasive procedures that provide limited functional insights into digestive processes.
Advanced digestive health monitoring technology represents a revolutionary shift in how we approach gastrointestinal disease management, particularly for conditions like IBS where symptoms fluctuate significantly. By collecting objective data directly from stool gases, these innovative systems provide unprecedented visibility into digestive function across the spectrum of GI disorders.
Diagnostic Challenges Across Gastrointestinal Diseases
Current Limitations in Digestive Disease Assessment
The path to effective management of gastrointestinal diseases is hindered by several diagnostic limitations:
- Colonoscopies and endoscopies provide structural information but miss functional patterns that occur between appointments
- Laboratory stool samples offer delayed snapshots rather than real-time gastrointestinal disease data
- Patient symptom diaries are subjective, inconsistent, and fail to capture the complex interplay of factors affecting digestive health
- Blood tests show systemic inflammation markers but lack specificity for gastrointestinal disease activity
- Limited correlation exists between structural findings and actual patient experiences with conditions like IBS
According to research published in the American Journal of Gastroenterology, up to 40% of patients with functional gastrointestinal disorders receive inadequate diagnosis and treatment due to these assessment limitations.
The Critical Need for Continuous Monitoring
Gastrointestinal diseases, especially functional disorders like IBS, fluctuate significantly based on numerous factors:
- Dietary triggers specific to each gastrointestinal condition
- Stress levels directly impacting symptom severity across digestive diseases
- Sleep quality influencing intestinal permeability and inflammatory processes
- Medication effects and supplement interactions
- Environmental factors including travel, seasonal changes, and routine disruptions
Without continuous monitoring, these crucial patterns remain invisible, making management of IBS and other gastrointestinal diseases a frustrating process of trial and error.
Scientific Classification of Gastrointestinal Diseases and Symptoms
From IBS to IBD: The Spectrum of Digestive Disorders
Gastrointestinal diseases span a wide spectrum of conditions with overlapping symptoms:
- Functional disorders like IBS (affecting 10-15% of the population)
- Inflammatory Bowel Diseases (IBD) including Crohn's disease and ulcerative colitis
- Malabsorption syndromes such as celiac disease and lactose intolerance
- Motility disorders including gastroparesis and chronic constipation
- Structural abnormalities like diverticulosis and hiatal hernias
Each condition presents unique monitoring challenges, but all benefit from objective assessment of digestive function.
The Bristol Stool Scale: A Universal Language for Digestive Health
The Bristol Stool Scale provides standardized assessment across gastrointestinal diseases:
- Types 1-2 indicating constipation-predominant conditions (including IBS-C)
- Types 6-7 showing diarrhea-predominant conditions (including IBS-D)
- Variable patterns reflecting mixed-type disorders or fluctuating disease activity
- Consistency tracking revealing gastrointestinal disease trends over time
- Objective measurement complementing subjective symptom reporting
Research in the Journal of Neurogastroenterology and Motility demonstrates that objective stool assessment significantly improves diagnostic accuracy across multiple gastrointestinal diseases compared to patient recall alone.
Focus on High-Impact Gastrointestinal Diseases
IBS: The Common but Complex Disorder
IBS affects up to 15% of the global population and significantly impacts quality of life through:
- Unpredictable symptoms creating anxiety and lifestyle limitations
- Digestive disruption affecting nutrition absorption and energy
- Limited treatment effectiveness with current management approaches
- High healthcare costs due to frequent medical consultations
- Social isolation caused by fear of symptom episodes
Inflammatory Bowel Disease: The Monitoring Challenge
IBD requires careful monitoring to prevent complications:
- Disease activity fluctuations between clinical visits
- Early detection of inflammatory flares before symptoms worsen
- Treatment efficacy assessment in real-time
- Nutritional impact tracking
- Complication risk assessment
Functional Dyspepsia and GERD: Upper GI Monitoring
Upper gastrointestinal diseases benefit from monitoring:
- Correlation between dietary choices and symptom patterns
- Medication timing optimization
- Lifestyle modification effects
- Nocturnal reflux episodes detection
- Barrett's esophagus risk assessment
Revolutionary Approaches to Gastrointestinal Disease Management
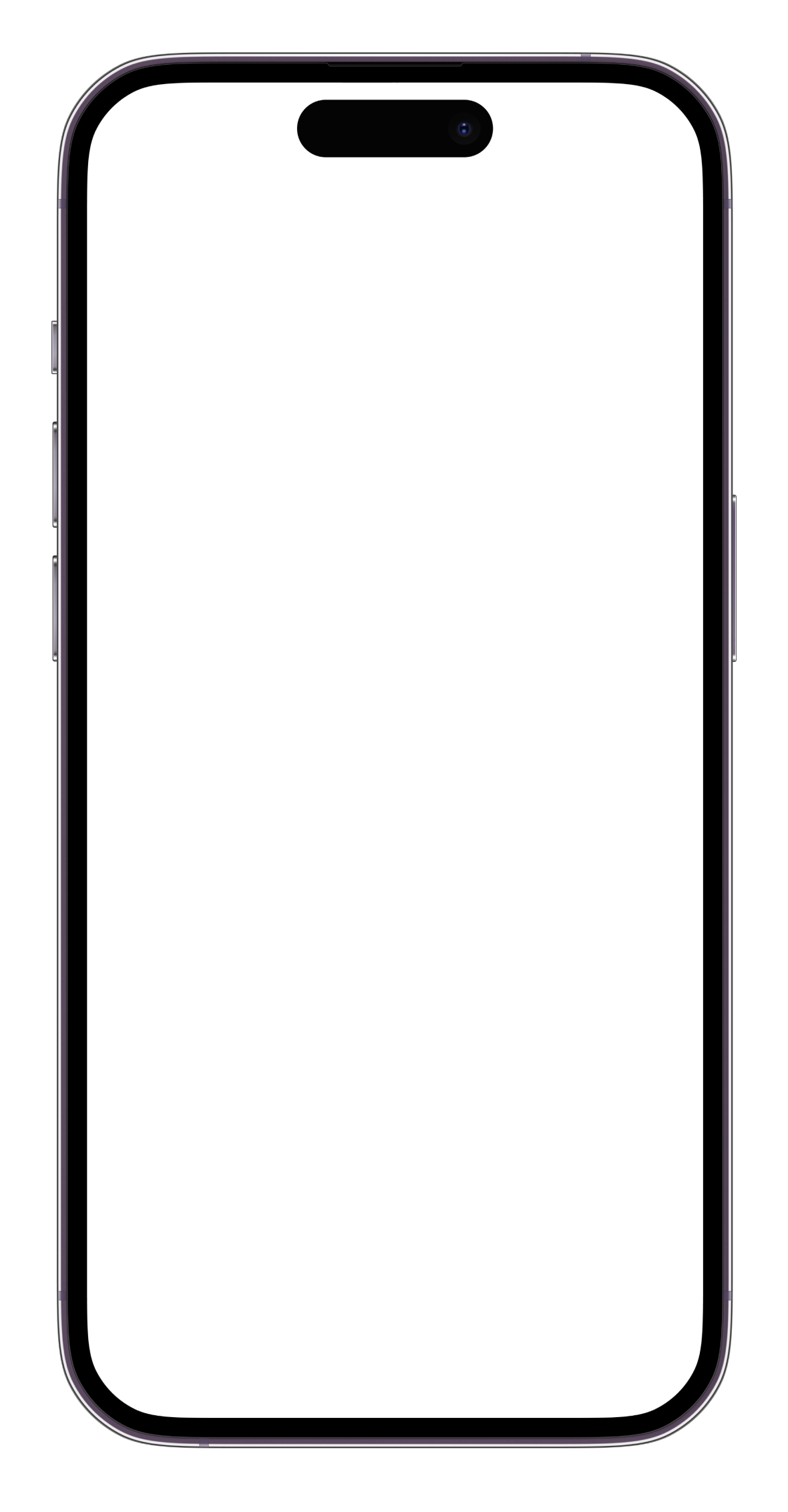
Real-Time Digestive Assessment
Continuous gut health monitoring provides critical insights across gastrointestinal diseases:
- Early warning indicators of potential flare-ups in IBS, IBD, and other conditions
- Objective trigger identification through molecular-level data
- Treatment response tracking showing symptom improvement
- Pattern recognition revealing personal digestive health rhythms
- Intervention timing for optimal symptom prevention
Volatile Organic Compounds (VOCs) in stool gas offer a scientific window into gut function that traditional diagnostic methods cannot provide. These gaseous compounds represent your microbiome's metabolic activity, providing insights into inflammation, dysbiosis, and functional patterns across gastrointestinal diseases.
Clinical Integration for Enhanced Digestive Care
Objective digestive health data facilitates improved management of all gastrointestinal diseases:
- More productive clinical discussions about symptom patterns and disease activity
- Evidence-based treatment modifications for digestive health optimization
- Shared decision-making based on real physiological data
- Better understanding of individual variations in gastrointestinal diseases
- Reduced healthcare visits through proactive symptom management
A study in Clinical Gastroenterology and Hepatology found that patients with access to objective monitoring data experienced 37% fewer emergency department visits for gastrointestinal disease complications.
Treatment Optimization Across Digestive Disorders
Healthcare providers can utilize digestive health monitoring to:
- Assess intervention effectiveness for symptom relief in IBS and other conditions
- Adjust medications based on objective digestive responses
- Track recovery progress during treatment protocols
- Identify concerning changes requiring immediate attention
- Personalize treatment approaches for individual gastrointestinal needs
Evidence-Based Management: The Future of Gastrointestinal Care
Research Integration for Digestive Disease Insights
Clinical practice benefits from comprehensive digestive health data:
- Large-scale population studies revealing patterns across gastrointestinal diseases
- Treatment outcome correlation with digestive biomarkers
- Predictive model development for disease management
- Clinical decision support through pattern recognition technology
- Quality improvement initiatives based on digestive health outcomes
A meta-analysis published in Gastroenterology demonstrated that objective biomarker monitoring improved treatment outcomes by 47% compared to symptom-based management alone across multiple gastrointestinal diseases.
Future Clinical Applications
Advanced digestive monitoring enables innovative approaches to gastrointestinal diseases:
- Precision medicine protocols tailored to individual digestive profiles
- Preventive care strategies based on early warning signs
- Remote patient monitoring for chronic gastrointestinal conditions
- Clinical trial enhancement through objective endpoints
- Population health insights from aggregated digestive health data
The Digestive Health Revolution: From Reactive to Proactive Management
The management of gastrointestinal diseases is evolving from a reactive, symptom-focused approach to a proactive, pattern-based strategy. By understanding the unique language of your gut through continuous monitoring, you gain unprecedented control over conditions ranging from IBS to IBD.
Let's face it, nobody enjoys discussing their bathroom habits, but everyone wants solutions to digestive problems. Advanced monitoring systems transform invisible data from your toilet into visible, actionable insights about your gastrointestinal health. This scientific approach to understanding what comes out of your body gives you the power to make informed decisions about what goes in.
Disease-Specific Applications
IBS Management Revolution
For IBS patients, continuous monitoring provides:
- Personalized trigger identification beyond generic elimination diets
- Prediction of symptom episodes before they occur
- Objective assessment of treatment efficacy
- Pattern recognition for lifestyle optimization
IBD Activity Tracking
For Inflammatory Bowel Disease patients, monitoring offers:
- Early detection of inflammatory flares through VOC patterns
- Medication adherence impact assessment
- Nutritional therapy effectiveness tracking
- Remission maintenance support
Functional Dyspepsia and GERD Management
For upper gastrointestinal conditions, monitoring systems can:
- Correlate symptom patterns with specific dietary choices
- Optimize medication timing for maximum effectiveness
- Track lifestyle modification impacts
- Identify patterns preceding symptom episodes
Recommended Resources for Comprehensive Digestive Health
Looking to deepen your understanding of gastrointestinal disease management? Explore these specialized topics:
- "Beyond IBS: Advanced Monitoring for All Gastrointestinal Diseases"
- "The Microbiome Connection: How Gut Bacteria Influence Digestive Disease Patterns"
- "Inflammatory Markers in Stool: What Your VOCs Reveal About Gut Health"
- "Digital Biomarkers: The Future of Gastrointestinal Disease Assessment"
- "Precision Nutrition Through Digestive Monitoring: Optimizing Diet for Your Unique Gut"
SNIFR is designed to provide insights about gut health patterns, not to diagnose or treat medical conditions. Individual results may vary as gut health is influenced by numerous factors including diet, stress, sleep, and genetics.
Other Posts
Be first to try SNIFR. Beta coming soon.
Join our waitlist to get notified when the app launches. Start understanding your gut health sooner.